Pain
Pain is a HUGE trigger word for many patients, and it’s one of the most important aspects of patient care that physical therapists deal with on a daily basis. Important in the world of pain is understanding that there is no way to directly measure pain, due to the billions of neurons and multi-faceted central and peripheral nervous systems. Physical therapists are the movement experts and conceptualizing what may or may not be contributing to a patient’s dysfunction is paramount. Understanding these concepts will make you a better therapist!
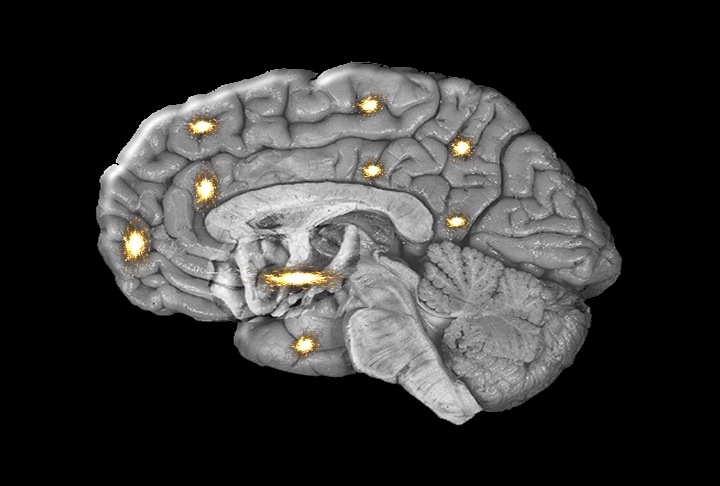
Pain Perception Regions of Brain

Unfortunately, physical therapists don’t always have the opportunity to evaluate an injury immediately after it happens. A patient may report to a clinic complaining of an injury that happened within the past few hours, days, or weeks. On the other hand, a patient may arrive at a clinic with symptoms that have progressed over many years. The timeline from injury onset to being seen by a physical therapist can make the diagnosis and prognosis rather complicated. A person’s pain profile may change over time. Findings at the onset may change upon reexamination, making accurate examination more difficult. Without witnessing an injury, or examining the individual at the onset of symptoms, a new grad physical therapist’s detective work must be broad. This requires that the clinician is meticulous when investigating the injury’s severity, irritability, nature, and stage. Outlined below is a quick look at how a newly graduated physical therapist can differentiate between a person with acute or chronic pain.
Acute Pain
Acute Pain is a direct response to incoming external/internal stimuli that is voraciously processed by your nervous system as a protective mechanism against further damage to the body. Acute pain can be helpful in diagnosing a problem. For example, if a patient comes to your clinic with severe sharp right lower quadrant pain localized to McBurney’s point and a fever, this is most likely presenting as appendicitis and requires possible surgical intervention (emergent referral). Furthermore, another patient comes to your clinic presenting with a non-contact knee injury (they planted their foot “wrong” and heard their knee pop with immediate swelling and pain) is likely an ACL sprain which requires a modification of physical activity to ensure proper healing of knee before surgery. These examples all show that a patient can present with acute pain that is essential for protection from further injury.
Acute musculoskeletal pain from injury or surgery will usually follow a predictable timeline of abatement within the population who take the proper precautions of going to physical therapy. Obvious complicating factors are success of surgery, severity of injury, coping mechanisms of the patient, adherence to exercise and protection protocols, use of assistive devices, financial resources, and psychological and social support.
Common Presentations of Acute Pain
•Less than 3 months in duration
•Sharp/throbbing/pulsing/electric/paresthesia/burning (peripheral/nociceptive/neurogenic pain systems) in quality
•Moderate to severe intensity at first and decreases predictably over time (based on type of tissue injury)
•Edema is common and also decreases predictably over time
•Pain disappears once healing is complete
•Mood tends to not change the patient’s complaints
•Pain provocation tests produce the patient’s initial complaints
•Pain is localized to site of injury or can present in standard referral patterns
•Results from something specific, such as an injury, or inflammation
•Discoloration is common such as ecchymosis and/or hematoma
•High disability scores at first, but scores decrease predictably (along with tissue healing, pain, and edema)
•Passive and active movement of body part produces the initial complaints and lessens when movement is complete
•Static and dynamic positions of body (such as standing, sitting, walking, lying, getting up from sitting, etc. ) change the quantity and quality of the pain predictably
Example – standing on a tibial shaft fracture (cleared for WBAT) will cause more pain than lying down
Chronic Pain
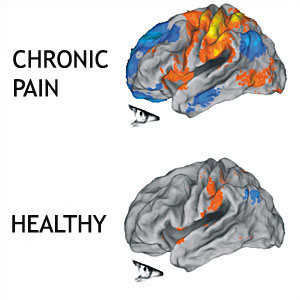
Defining when pain symptoms become chronic is always difficult (Macrae, 2001). Generally, pain is considered chronic when symptoms extend beyond the expected period of healing. There is no longer tissue damage. Often, the actual tissue damage has healed. Timelines of healing depend on which tissue was injured. In most cases, the healing process will finish in 3-6 months and the pain now has less to do with tissue damage or the site of the pain. The structure and chemistry of the nervous system are altered in the presence of chronic pain. Nociceptors sprout more nerve endings. Sensitivity thresholds are lowered. New nociceptors are grown. Chemicals are released at nerve endings that are inflammatory. The homunculus, for the painful region, can expand and “blur” into adjacent areas which can easily spread the sensation of pain by becoming more generalized in location (Wand et al., 2011). This is what makes dealing with acute and chronic pain completely different. Furthermore, if one approaches chronic pain with an acute pain strategy, one will struggle to be successful at reducing the patient’s pain.
Common Presentations of Chronic Pain
DISCLAIMER: First, you must try to rule out nefarious pathology that may be systemic in origin such as a malignancy, an infectious disease, or an autoimmune disorder.
Dramatization of complaints
Drug misuse
Dysfunction/disuse
Dependency
Depression
Disability
•Greater than 3 months in duration
•Pain symptoms become more generalized topographically and less localized to the site of injury or initial complaint
•Pain referral patterns that shift in location as well as intensity, frequency, and quality
•Pain that does not change with movement, rest, or over time
•Patients usually report pain as constant or continuous (less like to be intermittent)
•Mood or current psychological status tends to affect or worsen the pain complaints (Tang et al., 2009)
•Functional Measures and of percentage of disability indexes such as LEFS, DASH, Oswestry Neck and Back habitually show high disability
•Fear Avoidance Belief Questionnaire scores > 19 which correlate with greater incidence and prolonged bouts of chronic low back pain
•Pain Sensitivity Questionnaire can be used to measure general pain perception (pain perception outside the clinical pain site) in patients with chronic pain (Ruscheweyh et al., 2012)
References
References
 NewGradPhysicalTherapy.com The Largest Online Resource For New Grad Physical Therapists
NewGradPhysicalTherapy.com The Largest Online Resource For New Grad Physical Therapists